- 2.84 MB
- 2022-04-29 14:26:21 发布
- 1、本文档共5页,可阅读全部内容。
- 2、本文档内容版权归属内容提供方,所产生的收益全部归内容提供方所有。如果您对本文有版权争议,可选择认领,认领后既往收益都归您。
- 3、本文档由用户上传,本站不保证质量和数量令人满意,可能有诸多瑕疵,付费之前,请仔细先通过免费阅读内容等途径辨别内容交易风险。如存在严重挂羊头卖狗肉之情形,可联系本站下载客服投诉处理。
- 文档侵权举报电话:19940600175。
'子宫内膜癌治疗相关问题-妇产科课件
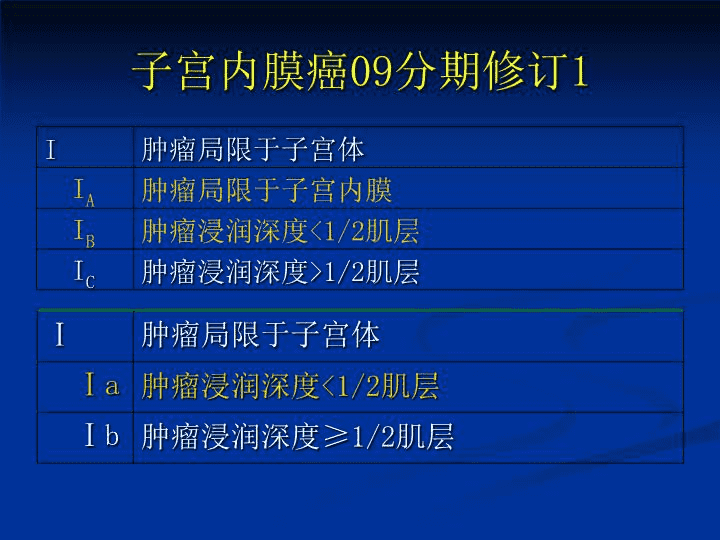
子宫内膜癌新分期子宫内膜癌淋巴结切除必要性子宫内膜癌子宫切除的范围
全国高等院校教材妇产科学乐杰主编林仲秋编写p275I期子宫内膜癌应行筋膜外子宫切除术及双附件切除术盆腔及腹主动脉旁淋巴结切除和(或)取样术下列情况之一,应行盆腔及腹主动脉旁淋巴结切除和(或)取样术可疑淋巴结增大宫颈受累CA125显著升高特殊组织类型癌灶累及宫腔面积超过50%低分化深肌层受累
CochraneDatabaseSystRev.2010Jan20;(1):CD007585.Lymphadenectomyforthemanagementofendometrialcancer.MayK,BryantA,DickinsonHO,KehoeS,MorrisonJUniversityofOxford,Women"sCentreNoevidencethatlymphadenectomydecreasestheriskofdeathordiseaserecurrencecomparedwithnolymphadenectomyinwomenwithpresumedstageIdisease.Theevidenceonseriousadverseeventssuggeststhatwomenwhoreceivelymphadenectomyaremorelikelytoexperiencesurgicallyrelatedsystemicmorbidityorlymphoedema/lymphocystformation.
JNatlCancerInst.2008Dec3;100(23):1707-16.Epub2008Nov25Systematicpelviclymphadenectomyvs.nolymphadenectomyinearly-stageendometrialcarcinoma:randomizedclinicaltrial.Rome,ItalyCONCLUSION:Althoughsystematicpelviclymphadenectomystatisticallysignificantlyimprovedsurgicalstaging,itdidnotimprovedisease-freeoroverallsurvival.
Lancet.2009Jan10;373(9658):125-36.Epub2008Dec16.Efficacyofsystematicpelviclymphadenectomyinendometrialcancer(MRCASTECtrial):arandomisedstudy.Collaborators(180)AmosC,BlakeP,BransonA,BuckleyCH,RedmanCW,ShepherdJ,DunnG,HeintzP,YarnoldJ,JohnsonP,MasonM,RuddR,BadmanP,BegumS,ChadwickN,CollinsS,GoodallK,JenkinsJ,LawK,MookP,SandercockJ,GoldsteinC,UscinskaB,CruickshankM,ParkinDE,CrawfordRA,LatimerJ,MichelM,ClarkeJ,DobbsS,McClellandRJ,PriceJH,ChanKK,MannC,RandR,FishA,LambM,GoodfellowC,TahirS,SmithJR,GornallR,Kerr-WilsonR,SwinglerGR,LaveryBA,ChanKK,KehoeS,FlavinA,EddyJ,Davies-HumphriesJ,HockingM,Sant-CassiaLJ,PearsonS,ChapmanRL,HodgkinsJ,ScottI,GuthrieD,PersicM,DanielFN,YiannakisD,AlloubMI,GilbertL,HeslipMR,NordinA,SmartG,CowieV,KatesmarkM,MurrayP,EddyJ,GornallR,SwinglerGR,FinnCB,MoloneyM,FarthingA,HanochJ,MasonPW,McIndoeA,SoutterWP,TebbuttH,MorganJS,VaseyD,CruickshankDJ,NevinJ,KehoeS,McKenzieIZ,GieC,DaviesQ,IrelandD,KirwanP,DaviesQ,LambM,KingstonR,KirwanJ,HerodJ,FianderA,LimK,HeadAC,LynchCB,BrowningAJ,CoxC,MurphyD,DuncanID,MckenzieC,CrockerS,NietoJ,PatersonME,TidyJ,DuncanA,ChanS,WilliamsonKM,WeekesA,AdeyemiOA,HenryR,LaurenceV,DeanS,PooleD,LindMJ,DealeyR,GodfreyK,HatemMM,LopesA,MonaghanJM,NaikR,EvansJ,GillespieA,PatersonME,TidyJ,IndT,LaneJ,OatesS,RedfordD,FordM,FishA,Larsen-DisneyP,JohnsonN,BolgerA,KeatingP,Martin-HirschP,RichardsonL,MurdochJB,JeyarajahA,LambM,McWhinneyN,FarthingA,MasonPW,KitchenerH,BeynonJL,HogstonP,LowEM,WoolasR,AndersonR,MurdochJB,NivenPA,Kerr-WilsonR,ChinK,FlynnP,FreitesO,NewmanGH,McNallyO,CullimoreJ,OlaitanA,MouldT,MenonV,RedmanCW,GeorgeM,HatemMH,EvansA,FianderA,HowellsR,LimK,CawdellG,WarwickAP,EustaceD,GilesJ,LeesonS,NevinJ,vanWijkAL,KarolewskiK,KlimekM,BlecharzP,McConnellD.
Hysterectomyandbilateralsalpingo-oophorectomy(BSO)isthestandardsurgeryforstageIendometrialcancer.Systematicpelviclymphadenectomyhasbeenusedtoestablishwhetherthereisextra-uterinediseaseandasatherapeuticproceduremedianfollow-upof37months(IQR24-58)191womenhaddied:88/704standardsurgerygroup103/704lymphadenectomygroup251Recurrentdisease107/704standardsurgerygroup144/704lymphadenectomygroup)
INTERPRETATIONnoevidenceofbenefitintermsofoverallorrecurrence-freesurvivalforpelviclymphadenectomyinwomenwithearlyendometrialcancer.Pelviclymphadenectomycannotberecommendedasroutineprocedurefortherapeuticpurposesoutsideofclinicaltrials.
子宫内膜癌淋巴结切除利与弊
争论“由来已久”!
早期:淋巴结转移率较低国内中山肿瘤:临床Ⅰ7.9%,Ⅱ8.6%,Ⅲ38.4%浙江肿瘤:临床Ⅰ4.4%,Ⅱ14%,Ⅲ34.8%国外StageⅠb(a)G1-2或IaG3:转移率0-2%StageⅠb(a)G3或Ic(b)G1:转移率16%-20%
早期:LND并未降低复发改善生存1996年10月到2006年3月意大利多个中心的514例术前FIGO分期为Ⅰ期子宫内膜癌患者随机分配接受盆腔淋巴结切除术(n=264)或者不进行此手术(n=250)“冲锋在前”的意大利研究
生存上没有差异5年DFS5年OS未接受淋巴结切除术81.7%90.0%接受淋巴结切除术81%85.9%
复发时间和复发率相似复发时间复发率(mth)(49mth)未进行淋巴结切除13mth33例(13.2%)淋巴结切除术者为14mth34例(12.9%)
复发部位相似
LND手术并发症明显增加在手术时间和住院时间上,两组有显著的统计学差异接受盆腔淋巴结切除术的患者有较高的早期和晚期术后并发症率,两组出现并发症的患者分别为81例和34例。
改变观念无容置疑子宫内膜癌治疗正朝个性化治疗发展已有充足证据证明Ⅰ期子宫内膜癌患者,淋巴结切除术不能带来任何生存获益。
特殊患者手术难度增加,风险增加肥胖高龄心血管疾病糖尿病
淋巴结真的可以不切除吗?LesionsitesandregionDepthofmyometrialinvasionCervicalinvasionExtrauterineinvasionornot,singleormultiplePathologicalgradeandclassificationLymphvascularinvasion(LVI)淋巴转移相关因素
病灶大小与淋巴结转移TumorSizeLNmets:2cm4%>2cm15%entireuterinecavity35%5-ysurvival:2cm-98%>2cm-84%entireuterinecavity-64%
建议有指征的行腹膜后淋巴结切除术
腹膜后淋巴结切除指征术前B超、MRI等估计深肌层受侵术前病理分级为G3术前临床分期II期以上术中探查腹膜后淋巴结可疑转移术中发现侵肌≥1/2术中发现宫腔50%以上有病灶累及子宫内膜浆乳癌、透明细胞癌等
一定要切除腹主动脉旁淋巴结吗?EurJGynaecolOncol.2007;28(2):98-102.PrinceofWalesHospital,Shatin,HongKongIsaorticlymphadenectomynecessaryinthemanagementofendometrialcarcinoma?75(46.0%)pelviclymphadenectomyalone88(54.0%)hadbothpelvicandaorticlymphadenectomy35(21.5%)nodalmetastasespositivepelvic26(16.0%)positiveaortic24(27.3%)Isolatedaorticmetastases17cases(19.3%)
35patientswithnodalmetastasesrecurrencedevelopedin15(42.9%)andallexceptonediedwithinfiveto50monthsTherecurrenceratewashigher(63.6%)amongpatientswithupperaorticlymphnodemetastasesallthosewhorecurreddiedofdiseasewithinsevento28months.
CONCLUSIONSaorticlymphadenectomyprovidesbothdiagnosticandtherapeuticvalueinthemanagementofendometrialcarcinomawithhighmetastaticrisk.
TodoYetal.Survivaleffectofpara-aorticlymphadenectomyinendometrialcancer(SEPALstudy):aretrospectivecohortanalysis.Lancet.2010Apr3;375(9721):1165-72671patientswithendometrialcarcinomasystematicpelviclymphadenectomy(n=325)pelvicandpara-aorticlymphadenectomy(n=346)INTERPRETATION:Combinedpelvicandpara-aorticlymphadenectomyisrecommendedastreatmentforpatientswithendometrialcarcinomaofintermediateorhighriskofrecurrence.
Ⅰ期子宫内膜癌子宫切除范围
33I期子宫内膜癌子宫切除范围:全子宫切除术?筋膜外子宫切除术?二者异同?次广泛子宫切除术?FIGO2009子宫内膜癌分期改变影响子宫内膜癌子宫切除范围的选择吗?局限于子宫的内膜癌手术选择争议:局限于子宫,宫颈累及?广泛子宫切除术?子宫切除范围值得探讨
内膜癌病变局限于子宫--手术方式DiseaselimitedtouterusMedicallyinoperableoperableTumordirectedRTTotalhysterectomyandbilateralsalpingo-oophorectomyLymphonodesdissectionpelvic+paraaorticThecurrentNCCNClinicalPracticeGuidelinerecommendspracticingradicalhysterectomyonlywhencervicalinfiltrationissuspectedonMRIorwhenconfirmedbycervicalbiopsy.2009NCCN
FIGO:筋膜外子宫切除术GOG2010:Womenwithendometrialcancersshouldundergototalabdominalhysterectomyandbilateralsalpingo-oophorectomy(TAH-BSO),pelvic/paraaorticdissection妇科常见恶性肿瘤治疗指南:筋膜外子宫切除术林巧稚妇科肿瘤学:全子宫切除术中国妇产科学(曹泽毅主编):筋膜外子宫切除术I期子宫内膜癌--手术方式
I期子宫内膜癌--手术方式GanToKagakuRyoho.1995Aug;22(9):1163-8.Totalhysterectomyisdoneforcasesofstage0,modifiedradicalhysterectomyforstageI,radicalhysterectomyforstageII,andradicalhysterectomycombinedwithresectionofthemetastaticlesionsforstageIIIandIVZhonghuaFuChanKeZaZhi.2002Feb;37(2):90-3.SurgicalmethodisnotthemainfactorinfluencedthesurviveofstageIendometrialcarcinoma.
为什么不行广泛或次广泛子宫切除术Mauro Signorelli,etal.GynecologicOncology2009ModifiedRadicalHysterectomyVersusExtrafascialHysterectomyintheTreatmentofStageIEndometrialCancerRecurrenceClassIhysterectomy(n= 263)ClassIIhysterectomy(n= 257)NOrecurrence231(87.8)228(88.7)WIthrecurrence32(12.2)29(11.3)DFSHR(95%CI)87.7%(1.0ref)89.7%(0.91)(0.55–1.51)OSHR(95%CI)88.9%(1.0ref)92.2%(0.77)(0.44–1.33)
筋膜外子宫切除术目的toensurethatthecervixisentirelyremoved适应症:子宫内膜癌,早期宫颈癌与全子宫切除术异同?定义?手术中要点?
筋膜外子宫切除术方法:Thepositionoftheuretersisdeterminedbypalpationwithoutfreeingtheuretersfromtheirbeds.Theparametriumistransectedmedialtotheureter,butlateraltothecervix,keepingtheparacervicalringintact.Theuterosacralandvesicouterineligamentsaretransectedclosetotheuterus.Thereisnoremovalofparacolposandaminimalpartofvaginaisresectedatfornixlevel.
病变累及宫颈手术范围的选择II期子宫内膜癌子宫切除范围首选广泛子宫切除术(II~III型子宫根治术)累及宫颈粘膜,现在归为I期,子宫切除范围?累及粘膜和间质如果应该选择不同的手术范围,如何术前鉴别诊断之?宫颈是否累及?是否间质浸润?术前诊断困难40分期改变带来的新问题
累及宫颈粘膜(I期)?OLD:IC差于IIANEW:II差于所有I期IIA期宫旁累及?宫颈癌早期手术范围如何识别粘膜累及还是间质浸润FIGO1988FIGO2009I期IAIBIC(56757)91%89%77%90%78%IIIAIIIBIIICIIIC1IIIC259%36%54%(3120)56%36%-57%49%累及宫颈粘膜(一期)?
诊断和鉴别宫颈粘膜累及还是间质浸润分段诊刮或宫腔镜检查宫颈管阴性宫颈上皮浸润I型子宫切除术MR局限于颈管内膜侵犯宫颈间质II或III型子宫切除术宫颈间质浸润
宫颈累及时子宫切除范围选择指南:广泛子宫切除术局限于子宫归为一类II期子宫内膜癌:筋膜外或广泛子宫切除术KOREA,JAPAN:Choosethesurgicalextentofhysterectomythroughtheirowndispositionanddonotstrictlyadheretheresultsofpreoperativeevaluation.JAPANESEgroupmorethan70%ofinstitutesneverperformRHwithoutregardingthepreoperativestatusofcervicalinvolvement(Watanabe)NORTHAMERICAN:20-30%center
II期子宫内膜癌RH手术的必要性II期子宫内膜癌手术方式的选择
II期子宫内膜癌RH手术的必要性Depthofmyometrialinvasionandpelvicorparaaorticlymphnodepositivityweresignificantlycorrelatedwithparamatrialinvolvement.Ofthe19patientswithpelviclymphnodemetastasis,8patients(42.1%)hadconcomitantPMI.Conversely,ofthe10patientswithPMI,8(80.0%)hadlymphnodemetastasis.
'
您可能关注的文档
- 最新婴幼儿生理的特点 ppt课件PPT课件
- 最新婴幼儿牛奶蛋白过敏的诊治ppt课件PPT课件
- 最新婴幼儿肺动脉瓣狭窄的介入治疗及疗效影响因素分析课件PPT课件
- 最新婴幼儿运动技能训练 ppt课件PPT课件
- 最新婴幼儿长段输尿管狭窄的治疗PPT课件PPT课件
- 最新子午流注十二时辰 ppt课件PPT课件
- 最新子午流注讲稿课件PPT课件
- 最新子宫内膜癌Medometrialcacinoma课件PPT课件
- 最新子宫内膜癌的化疗-妇产科课件PPT课件
- 最新子宫内膜癌的筛查策略——子宫内膜细胞学的应用-妇产科课件PPT课件
- 最新子宫内膜癌诊治面临的问题与挑战-妇产科课件PPT课件
- 最新子宫内膜癌盆腔淋巴结转移特征及与预后关系的研究-妇产科课件PPT课件
- 最新子宫动静脉瘘超声诊断ppt课件PPT课件
- 最新子宫畸形课件PPT课件
- 最新子宫肌瘤 Myoma of uterus-妇产科课件PPT课件
- 最新子宫肌瘤教学查房ppt课件PPT课件
- 最新子宫肌瘤课件PPT课件
- 最新子宫肿瘤-妇产科课件PPT课件